Drugs and Current Research
Herceptin
Herceptin, or Trastuzumab, acts by blocking Human Epidermal Receptor 2 (HER-2) proteins on the surface of breast cancer cells.
Normally breast cells express levels of HER-2, which receive signals telling the cells to grow and divide. However, in the case of HER-2 positive breast cancer, the HER-2 gene is over expressed. Consequently too much HER-2 is present on breast cancer cell surfaces, making the cancer grow rapidly and become aggressive.
A HER-2 positive breast cancer may stand less chance of responding to other breast cancer treatments due to its aggressive nature. Herceptin inhibits HER-2 receptors on the cancer cells, preventing the cells from receiving growth signals, thereby helping reduce the spread of the cancer. It is used in cases of metastatic HER-2 positive cancer, or in conjunction with chemotherapy to reduce the chance of further spread.
A major side effect of Herceptin treatment is that the heart muscle can weaken. Doctors will monitor heart function when treating a patient with Herceptin, and treatment will immediately be discontinued if the health of the patient is being compromised because of Herceptin.
Also known by the chemical name Bevacizumab, Avastin is used in the treatment of HER-2 negative metastatic breast cancer. It aims to prevent angiogenesis of the tumour, that is, it stops new blood vessels from forming in and around the tumour. These blood vessels would otherwise cause the tumour to grow further.
Avastin is to date the only available drug which works in this angiogenesis-targeted way.
A study in 2005 conducted by the National Cancer Institute reported that patients who were given Avastin in combination with chemotherapy were less likely to see a progression in their cancer than those who received chemotherapy only.
Avastin is not yet the standard drug given to the majority of breast cancer patients. Results are promising, however, one study reported that tumours shrank in 63.1% of breast cancer patients.
Side effects of the drug can range from nosebleeds and fatigue to low white blood cell count and hypertension.
Ta moxifen is a selective oestrogen receptor modulator - it acts to lower the effects of the hormone oestrogen on the breast cancer cells. It attaches to the oestrogen receptors on the surface of the cells in order to prevent the binding of oestrogen molecules.
moxifen is a selective oestrogen receptor modulator - it acts to lower the effects of the hormone oestrogen on the breast cancer cells. It attaches to the oestrogen receptors on the surface of the cells in order to prevent the binding of oestrogen molecules.
If a breast cell contains a DNA mutation that causes it to become cancerous, oestrogen can further exacerbate its growth- in turn this can lead to uncontrolled differentiation of the cells, which can lead to cancer.
Selective oestrogen receptor modulators such as Tamoxifen are specific a particular target tissue-it only acts upon breast cells. It prevents the genes which cause cell proliferation from being switched on.
Tamoxifen is primarily used after surgery to reduce the risk of recurrence. It can also be used in the treatment of metastatic breast cancer to help reduce the cancer spreading.
Tamoxifen has been shown to decrease the rate of breast cancer recurrence by 40 to 50%. It also halves the risk of the cancer spreading from the breast of origin to the other one.
The most common side effects associated with Tamoxifen treatment are hot flushes, fatigue, headache and mood swings. Other more serious symptoms which are less likely include dizziness and chest pain- in which case a doctor will review and possibly reconsider the treatment options.
Image courtesy of https://www.flickr.com/photos/sergiop/3790165426/ under a Creative Commons license.
 Current Research
Current Research
BRCA1 and BRCA2
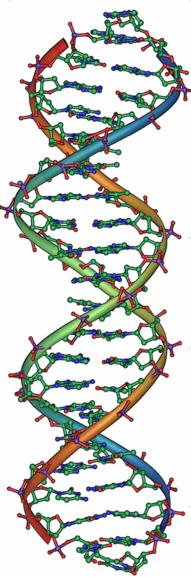
BRCA2 has been shown to interact with a gene known as Rad51. In cases of DNA damage, Rad51 is involved in a process called homologous recombination- a form of DNA repair. Mutations in BRCA2 can lead to cancer because the relationship between the gene and Rad51 is not functioning as it should, so the normal process of homologous recombination becomes inefficient.
In 2007, research was conducted by scientists at the Abramson Family Centre Cancer Research Institute of the University of Pennsylvania, which showed that the mutations that arise in BRCA1 cause the protein to be inefficient at binding to another protein called Rap80. As a result, DNA damage in the genome that would normally be recognised by BRCA1 is no longer recognised. Accumulations in this damaged DNA in breast cells leads to breast cancer.
Single nucleotide polymorphisms (SNPs) on chromosome 5p12 have been discovered which heighten the risk of breast cancer. At this site resides a gene called FGF10, which is known to be involved in the formation of breast cancer. Amplification of FGF10 is found in 10% of all breast cancers.
In 2010 genes implicated in breast cancer were found at 12 specific locations in the human genome. These 12 positions, or loci, accounted for about 5% of all cases of hereditary breast cancer. One gene of special significance was RAD51L, which encodes a Rad51 homologue protein. This protein is involved in the repair of damaged DNA, and a mutation in this gene would mean the cell is no longer able to repair the damage-potentially leading to cancer developing.
Image courtesy of https://commons.wikimedia.org/wiki/File:DNA_double_helix_45.PNG Image is in the public domain and is thus free of any copyright restrictions.
Permission to use BRCA1 and BRCA2 video was granted by Kim Tharaldsen - Product Manager, BRACAnalysis
